Our Amazing Design
Thanks to growing interest in user-friendliness, operational efficiency, and lower environmental impact, many modern products are advancing impressively. But nothing comes close—not even a little—to the sophisticated-yet-simple collection of nearly 40 trillion self-running, self-replicating, and self-repairing cells that we call the human body.
Since it’s packaged so neatly and works so efficiently, it’s easy to forget how impressive the human body really is. If you’re in pain, it’s even easier to forget that each of our 40 trillion cells (some say up to 100 trillion!) will do everything it can, in virtually any situation, to help us live and thrive.
Amazingly, our 200 types of human cells organize themselves into highly capable systems that make it easy for us to sense and control—or not, whichever is best—our various bodily actions, reactions, and behaviors. Without complaint, our cells sign up for internal work, face the outside world, or support transitional areas. As they interweave to integrate physical, mechanical, electrical, and chemical laws, they skillfully build a complete product responsive to the loads we place upon it. What’s more, if we’re at risk, our cells, parts, and systems will signal a warning or simply act on their own to minimize danger and damage.
Our digestive system in particular is a remarkably elegant structure designed to acquire nutrients and empower our cells to do their best work. It humbly accepts and processes anything we put into it, rejecting only the most detectably hazardous substances. So rather than being an object of disdain or disgust, our personal power plant—including the last six or seven inches that make up our anorectal area—is a marvel at every turn, and deserves a closer look.
In this section, I provide a few sketches that emphasize function over anatomical accuracy. To keep things simple, I leave out some parts, so if you’re technically-minded, be sure to review a good medical reference for the whole story.
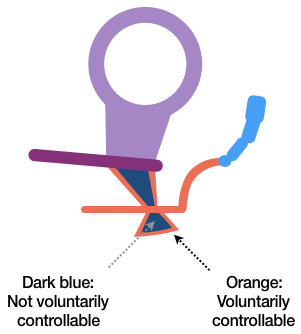
In some of my sketches, I use a bow tie-like shape to indicate body openings or internal sphincters. Items that can be controlled voluntarily are colored orange, those that cannot are colored dark blue or green (see Figure 1).
Two more suggestions:
First, if you look online for information about the GI tract, you might find a surprising variety of names, definitions, details, and debate—even in professional literature. So if you’re really interested in technical accuracy, I suggest asking a trusted medical provider for recommended resources.
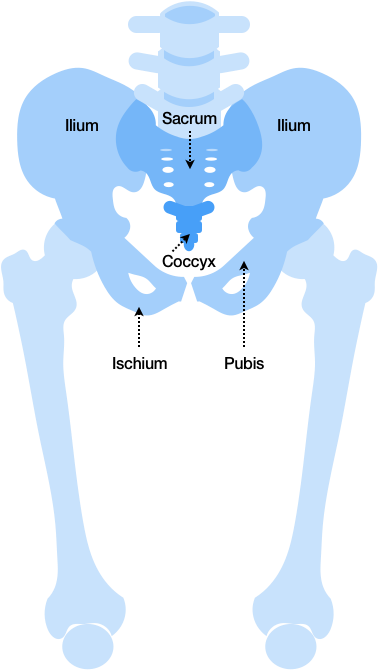
Second, avoid getting overwhelmed by names that sound strange or esoteric. “Sphincter” just comes from a Greek word that means “bind tight”, which is the same root word in “sphinx”, a mythical creature said to guard the gates of ancient cities. “Rectum” is Latin for “straight (intestine).” “Coccyx” comes from the Greek word for “cuckoo” because its shape resembles a cuckoo bird’s bill, and the area around the “pectinate line” looks a little like a rooster comb, so it’s described by a version of the Latin term (pecten) for “comb” or “rake.” Moreover, some modern-sounding terms actually reflect long-past ideas, such as the “sacrum” (sacred bone), called such based on the belief that one’s soul resides there.
So let’s start with the original you tube. For clarity, here’s our digestive tract presented in simple, functional terms (Figure 2):
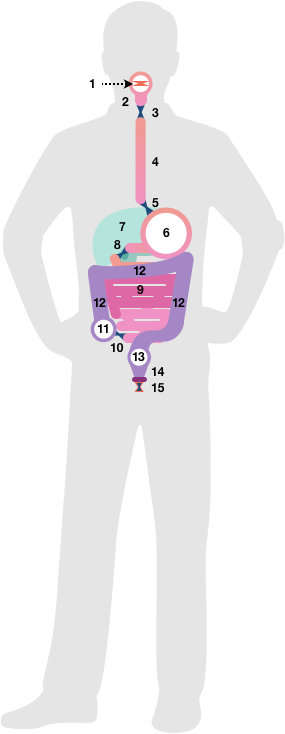
- Entry doors (user-controllable)
- Cutter/grinder with funnel
- Automatic door #1
- Elevator (going down)
- Automatic door #2
- Mix tank
- Chemical plant and refinery
- Automatic door #3
- Extraction pipeline #1
- Automatic door #4
- Staging area
- Extraction pipeline #2, including up elevator, conveyor belt, and down elevator
- Storage area
- Exit funnel
- Exit doors (partially user-controllable)
Here’s the same overview with common anatomical terms:
- Lips
- Mouth (or “Oral cavity”) and Pharyngeal Muscle Complex
- Upper Esophageal Sphincter
- Esophagus
- Lower Esophageal Sphincter (also called the “Cardiac Sphincter”)
- Stomach
- Liver, Pancreas, and Gall Bladder
- Pyloric Sphincter
- Small Intestine (Duodenum, Jejunum, Ileum)
- Ileocecal Valve
- Cecum
- Large Intestine (Ascending, Transverse, Descending, and Sigmoid Colon)
- Rectum
- Anal Canal (shown with Puborectalis muscle in place)
- Anal Sphincter Complex, including Internal (automatic) and External (user semi-controllable) Anal Sphincters
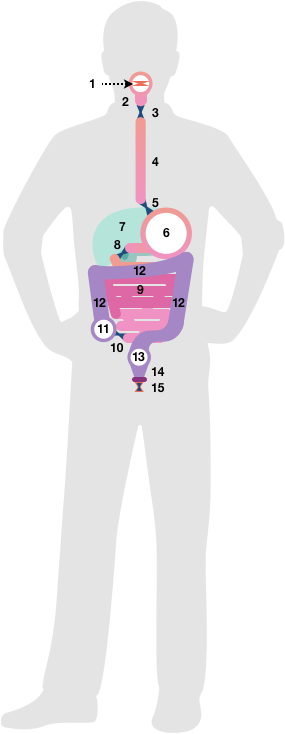
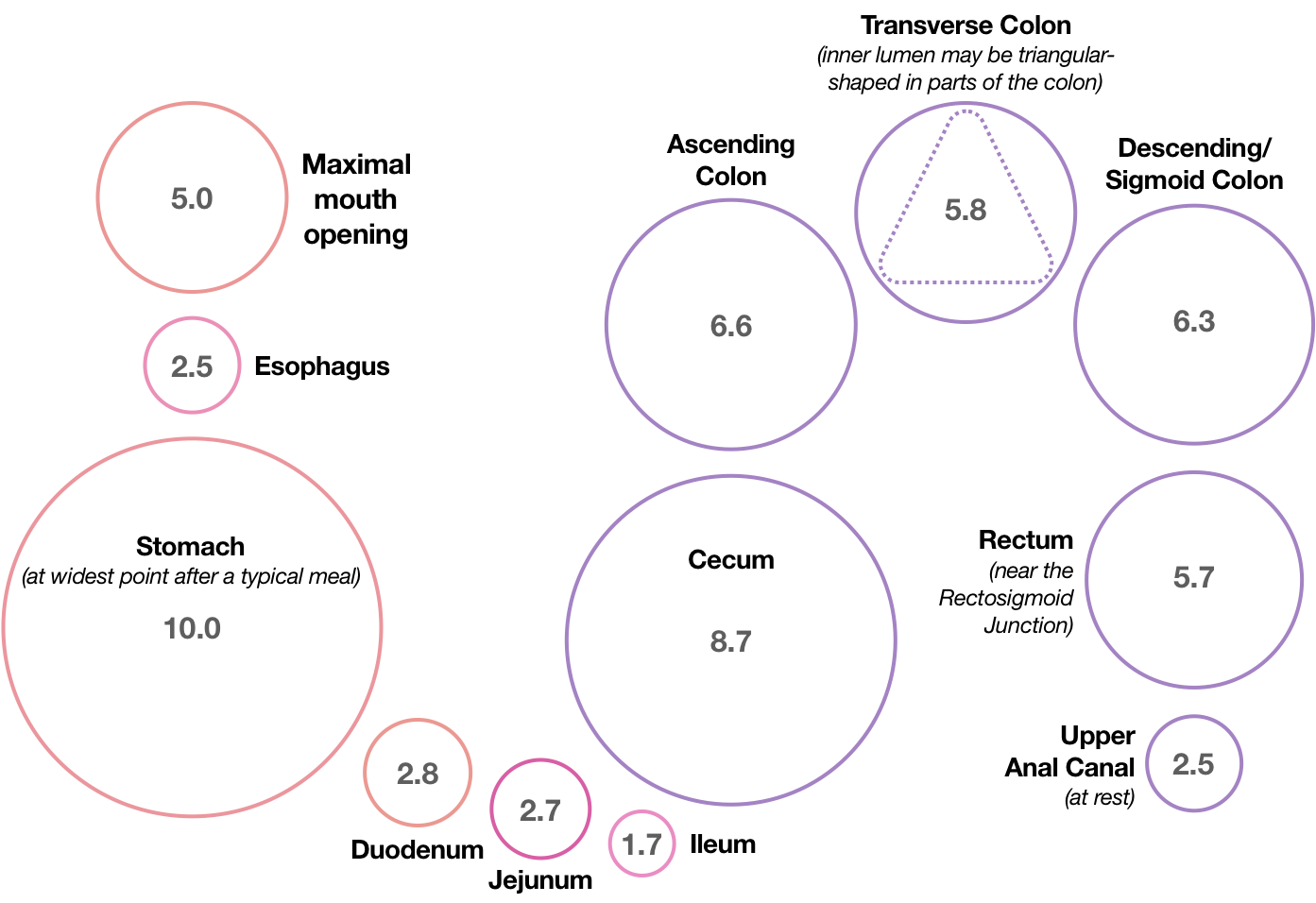
Since we’re talking tubes, here are the diameters of various inner hollow pipeline spaces, technically called a tube’s lumen, measured in centimeters for an average adult male. For those who haven’t adopted the metric system, one centimeter is about 3/8 inch. (Figure 4; not actual size):
Next, let’s look at a “subway map” of our GI tract, which is a common design technique used to show general pathways instead of detailed routes (Figure 5):

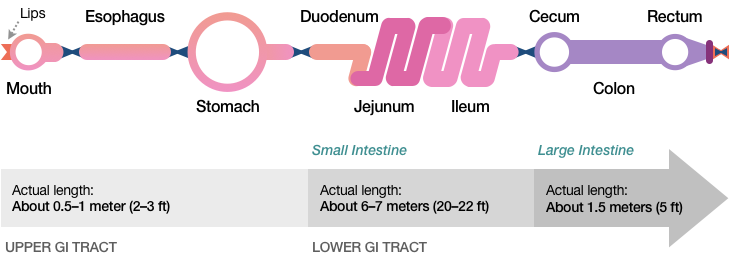
Here’s the same subway map view with average lengths for the Upper GI Tract (Esophagus to Stomach) and the two main parts of the Lower GI Tract—the Small Intestine and the Large Intestine (Figure 6):
Here’s the same view with our various digestive sphincters clearly marked, most of which perform their functions automatically (Figure 7):
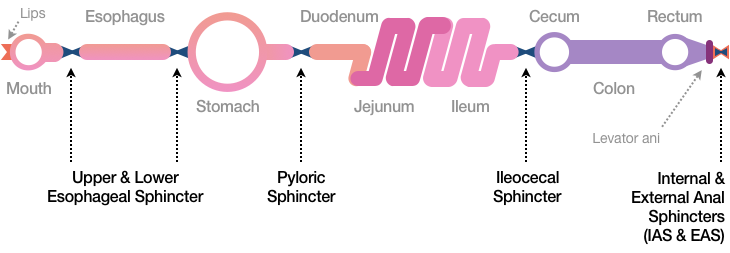

Speaking of sphincters, our bodies contain more than 60 types, almost all of which operate automatically (including millions of precapillary sphincters). Among our most user-controllable sphincters is the External Anal Sphincter (EAS), which can be likened to the iris of a cat’s eye in that it widens the anal canal into a circle but narrows it into a slit (Figure 8).
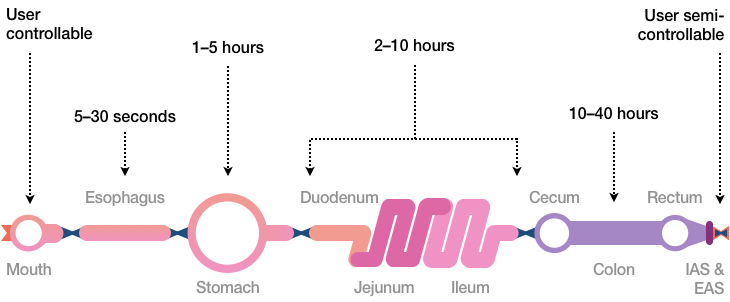
Total digestion time through the GI tract varies based on many factors, but here are some typical food transit times for an average adult (Figure 9):
So how does food move through the GI tract? To get a basic answer, let’s look briefly at tube construction.
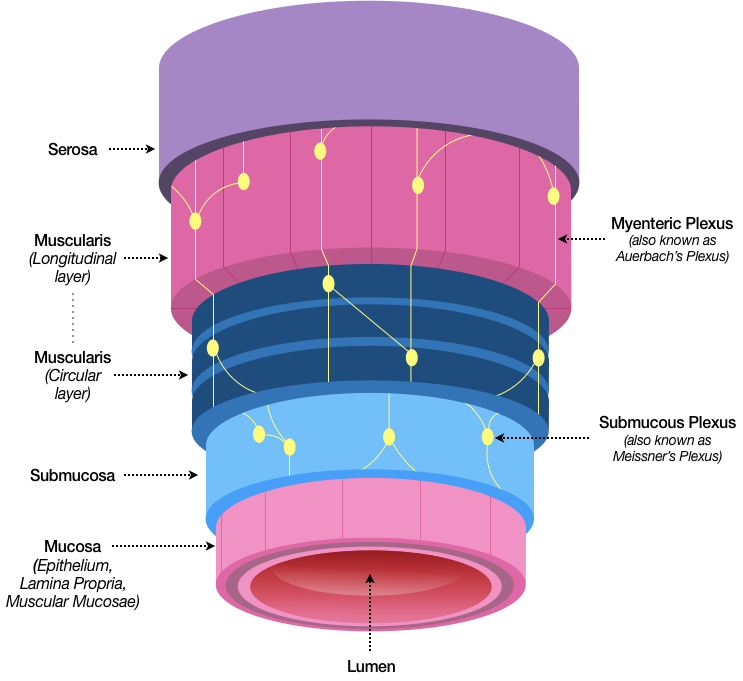
Our digestive tube material, anatomically called the gastrointestinal wall, contains an astounding number of components, yet is only about 1–5 millimeters thick, so in this sketch (Figure 10) I’ve sacrificed accurate proportions in favor of showing its main features. I’ve also left out some very powerful parts, such as goblet cells (which secrete the clear, antiseptic mucus necessary for our protection and survival), villi (which dramatically increase the surface area available to absorb nutrients), and lymphatic tissue (which helps circulate 4–5 liters of essential lymph fluid through our bodies daily), not to mention many types of cells, tissues, glands, veins, and other items that make our GI tract so effective at its job.
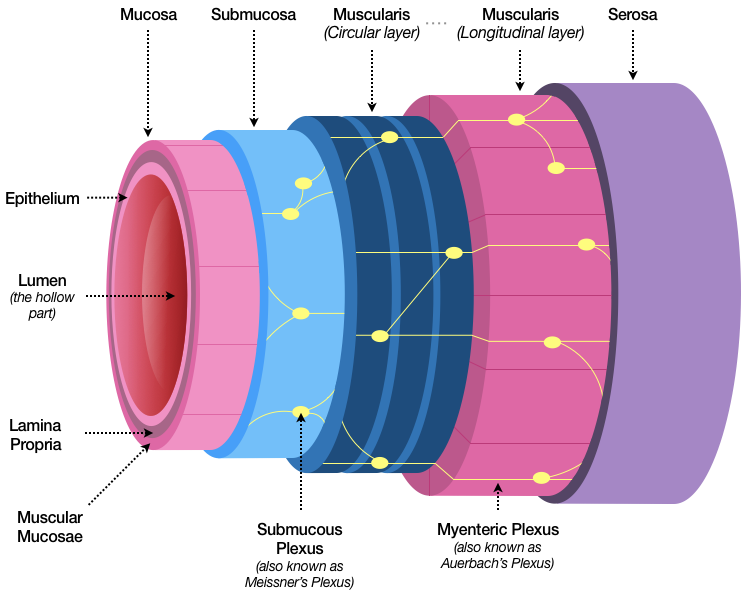
The four main features of the gastrointestinal wall are arranged in layers, and include the mucosa, submucosa, muscularis, and serosa. Key details:
- The mucosa (from Latin “slippery, slimy”) is the innermost series of layers, and includes the epithelium (the surface closest to the hollow tube, or lumen), the lamina propria (or “basement membrane”), and a thin layer of muscle called the muscular mucosae, which is present from the esophagus to the upper rectum, and which provides agitation (think washing machine) to help contents in the lumen better interact with the nutrient-absorbing epithelium.
- The second layer is the submucosa, which helps bind the mucosa to the third layer. Among other items, a network of nerves called the submucous plexus (also called Meissner’s plexus), runs throughout the submucosa.
- The third layer, the muscularis (or “tunica muscularis”, or simply the “muscular layer”) is also a series of layers, including an inner layer of circular muscle and an outer layer of longitudinal muscle. The muscularis contains a network of nerves called the myenteric plexus (or Auerbach’s plexus) and pacemaker cells (called myenteric interstitial cells of Cajal) that automatically help relax and contract the circular and longitudinal layers in a highly coordinated way. In the colon, the longitudinal layer separates into three bands that merge back together near the rectum; these work together with the circular layer to keep waste material moving forward while inhibiting unwanted back flow.
- The final layer, the serosa (or serous membrane), is a combination of connective tissue, epithelium, and lubricating fluid that helps reduce friction from muscle movement.
So how do these features get food moving? Along with connections to our autonomic (involuntary) nervous system, the 500 million neurons that make up our enteric nervous system—a mesh-like neural network so complex it’s sometimes called our “second brain”—are embedded in the submucous and myenteric plexuses. Responding to a variety of inputs, our autonomic and enteric nervous systems govern a basic electrical rhythm made by the pacemaker cells in the muscular layers to coordinate contraction and relaxation, as well as to control contraction frequency, which varies in different parts of the GI tract. Other electrical and chemical features help regulate contraction strength and timing.
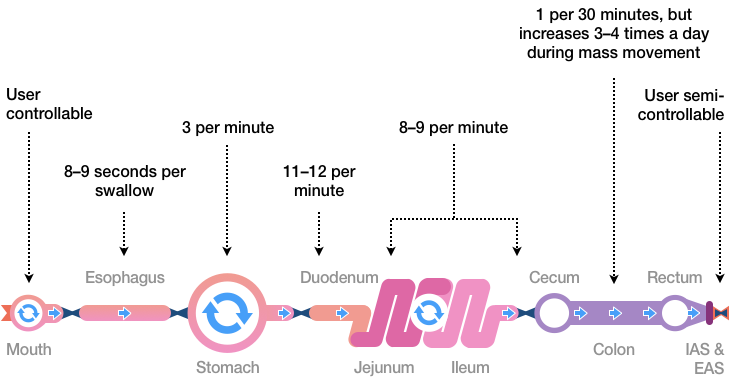
Different contraction types, in turn, help move and digest food. Peristaltic waves (Latin for “wrap around”) propel food forward. Segmentation contractions move tube contents back and forth, which assists digestive mixing and absorption. Food ultimately moves forward, and three to four times a day—often shortly after eating a meal—strong, sustained colon contractions called a mass movement push water, electrolytes, undigested food residue, and a small amount of other wastes toward the rectum. Here are some common timings for these various waves, contractions, and movements (Figure 11):
With that basic understanding of our GI tract, it’s easier to follow the food as we head toward the pelvic floor and anorectal area.
So how does food digestion work? In a very simplified way, like this (Figure 12):
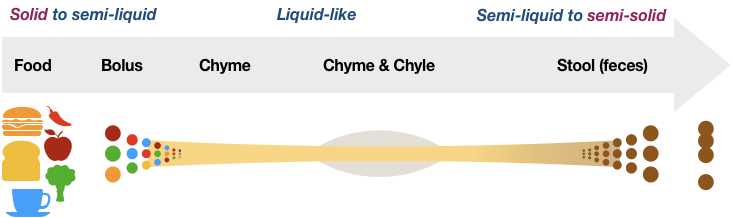
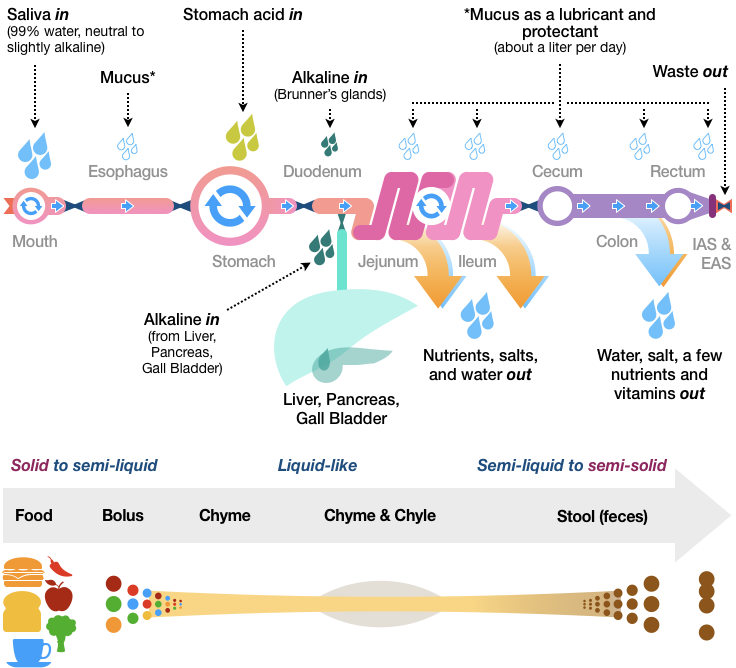
Under normal conditions, food and drink items are split into small, easily movable quantities. Fluids are added to create a liquid-like slurry optimized for nutrient absorption. After most nutritious value has been extracted, the GI tract recovers water and electrolytes, making waste material easier to store and excrete.
It’s a model of efficiency. On average, about 9.5 liters of fluid enter the small intestine each day. Since only about 2.5 liters come from ingested fluids and food, approximately 7 liters come from fluids already in the body. The small intestine absorbs 9 liters of fluid, which means that only about 500 mL (2 cups) enters the large intestine. Once there, an additional 350 mL gets absorbed, leaving only about 150 grams of material (about a third of a pound) to exit as waste. Everything else is absorbed, retained, or recycled!
Here are the details: Mouth action, assisted by slightly alkaline saliva, turns food into small packets, each of which is called a “bolus” (Greek for “clod”). The next step, swallowing (or “deglutition”), starts voluntarily, but automatic reflexes quickly take over: after passing the throat, each bolus enters the esophagus (normally collapsed until needed) through the upper esophageal sphincter. GI tract muscles then constrict and relax in rhythm, creating one-way peristaltic waves that move the bolus down the esophagus to the lower esophageal sphincter, and then to the stomach.
Once in the stomach, the contents of each bolus mix and combine with other fluids, including powerful acids. After that, the now pulpy acidic fluid, called chyme, moves into the small intestine.
Alkaline secretions in the duodenum reduce the chyme’s acidity. Segmentation contractions churn and mix the chyme. Nutrients start getting absorbed into the bloodstream, and a milky fluid of fat droplets and lymph—chyle—drains from the small intestine into the lymphatic system. The chyme, meanwhile, makes its way through the nutrient-absorbing jejunum and ileum, and at the bottom of the route enters the cecum through the ileocecal valve.
The material is then moved through the ascending, transverse, descending, and sigmoid (“s-shaped”) colon. Water, salt, and some vitamin extraction occurs in the large intestine, as does fermentation, thanks to the action of more than 700 varieties of almost 100 trillion bacteria. Now semi-solid waste, the material gets moved toward the rectum by occasional mass movements.
Let’s briefly pause here to see how the entire process works. In this diagram (Figure 13), I’ve loosely mapped food processing to our GI tract’s workflow:
Now that we have a basic overview of the digestive process, it’s time to move toward the exit. But before we do, it’s good to know where we’re headed.
The pelvic region is an amazing junction of design and engineering. Shaped like a bowl, the pelvis, sacrum, and coccyx serve to support and protect many crucial aspects of our anatomy through their complex yet wondrous shapes. An area of study in its own right, pelvimetry (or pelvic geometry) has traditionally been divided into four kinds—android, anthropoid, gynecoid, and platypelloid—and at times has been used to determine the type and style of child delivery for pregnant women. Having never thought about my own pelvimetry before, I found it interesting to explore the pelvic skeletal structure with my 3D anatomy app. Among other insights, doing so helped me appreciate how well-sited our anorectal area truly is. This sketch (Figure 14) shows a flat, foreshortened version of our pelvic area, and hardly does it justice.
If you check other resources for a more accurate picture of the pelvic and anorectal region, it’s helpful to know that though male and female muscles are similar, their configurations are different. For example, the external anal sphincter, as shown in this sketch (Figure 15), varies considerably by gender.
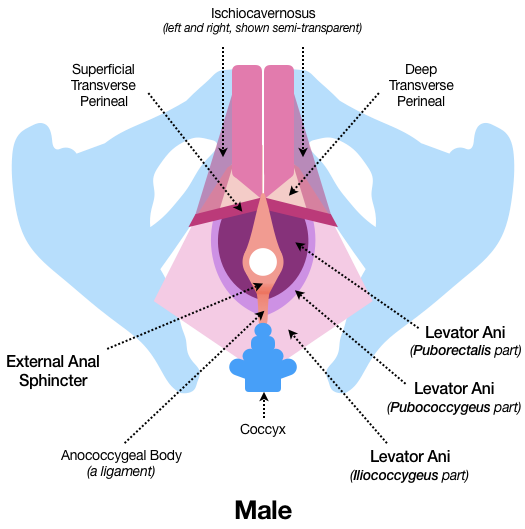
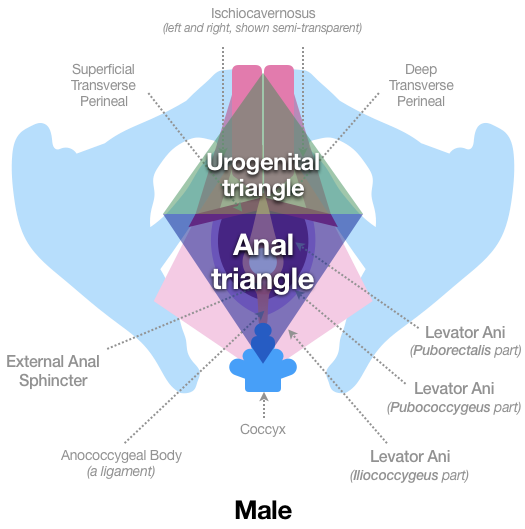
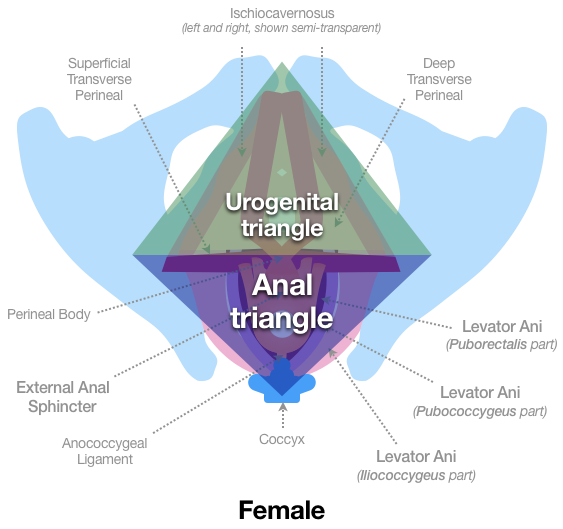
The muscles of the pelvic floor are likewise configured to accommodate the unique needs of male and female anatomy. Along with the pelvic bones, these first two sketches (Figures 16, 17) show the male configuration as seen from the feet and looking toward the head. From this perspective, it’s easy to see why the pelvic floor is often described as two triangular regions, the urogenital triangle and the anal triangle, which together form a diamond:
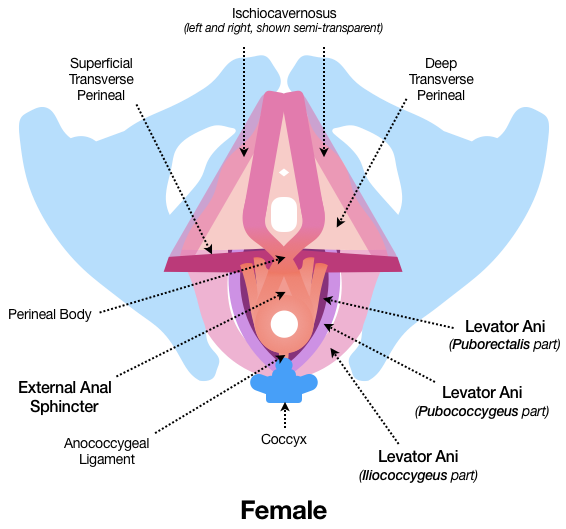
The female version from the same vantage point shows different muscular configuration and positioning of parts (Figures 18, 19). Similar to the male version, the external anal sphincter connects to the coccyx with the anococcygeal ligament, which is a strong fibrous band:
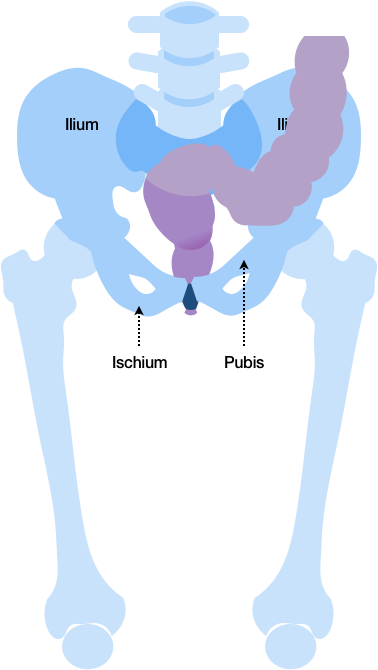
This next sketch (Figure 20) shows how the pelvic region makes an ideal protective enclosure for temporary waste storage. (By the way, don’t confuse the ilium of the pelvis with the ileum of the small intestine.)
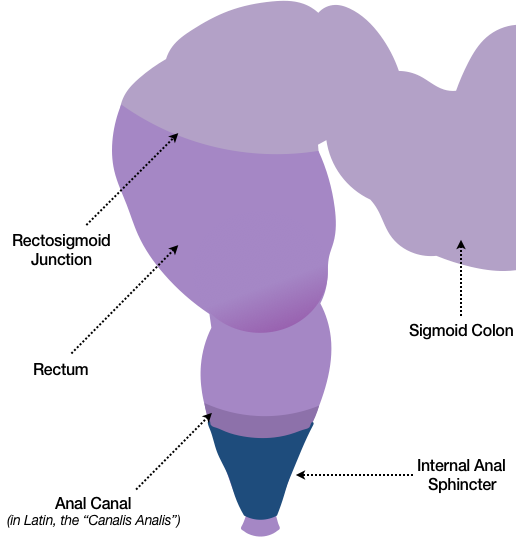
Isolating the non-skeletal features shows the need for muscular support, which is partially provided by the pelvic floor. Shown in the following sketch is the sigmoid colon, rectosigmoid junction, and anal canal with the internal anal sphincter highlighted in dark blue (Figure 21):
Many muscles, muscle groups, and other features converge in the pelvic region as well, but for our purposes, in the following sketch (Figure 22) we’ll isolate the fan-shaped levator ani, which is often shown as a muscle made of three parts: the iliococcygeal part, the pubococcygeal part, and the puborectalis part. Also shown (in orange) are two of three parts of the external anal sphincter: the deep part and the superficial part (the third part, the subcutaneous part, is not depicted here).
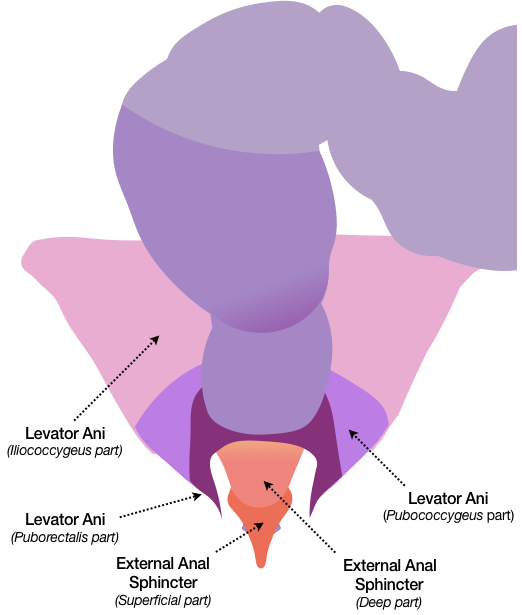
Figure 23 shows a simplified side view of the entire mechanism (male) in situ:
A schematic side view (male version) shows how the levator ani wraps around the rectum and anal canal (Figure 24). Though anatomically different, female functionality of the IAS, EAS, and Levator Ani is similar.
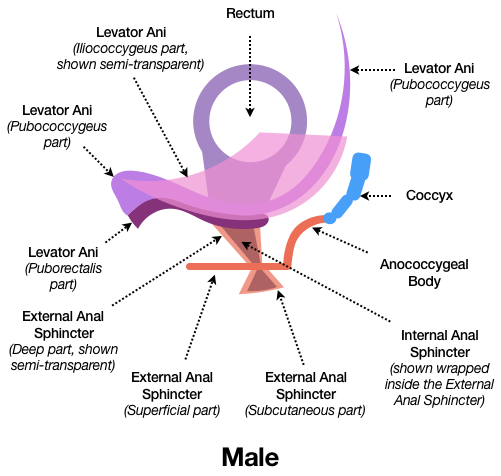
This next sketch removes the iliococcygeal and pubococcygeal parts of the levator ani, simplifies the puborectalis, and takes a cross-section view of the external anal sphincter to help illustrate the mechanism (Figure 25). Using this simplified view, the act of waste removal may be easier to understand.
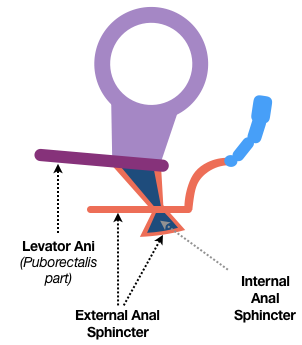
Like the internal and external anal sphincters, the puborectalis muscle is normally under gentle tension and holds the rectum at about an 80–90 degree angle. As stool fills the rectum and the rectal walls stretch, natural sensors signal fullness, and the puborectalis relaxes. As the rectum responds, its angle widens and stool moves down the anal canal, causing the internal anal sphincter to automatically relax and the external anal sphincter to automatically constrict (Figure 26).
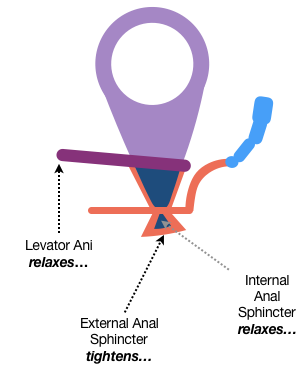
When it’s go time, the external anal sphincter relaxes, the rectum shortens, peristaltic waves move stool outward, the sphincters pull up over the exiting material, and the waste material gets completely released (Figure 27).
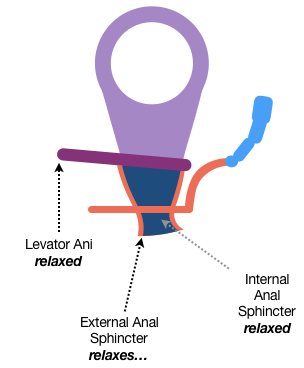
Once defecation is done, the sphincters and puborectalis return to a state of gentle tension (or “tone”) to close the doors and await the next passage.
Having reached the end of the line, it’s time to backtrack a bit and look more closely at the anorectal junction and the anal canal. Before we do, recall that we’re still talking about the same basic tube structure already described. By orienting our earlier sketch vertically, we begin to see how the main features of the gastrointestinal wall become the anal canal (Figure 28).
We’ll start with a cross-section of the tube and its passage to exterior skin, and then add more parts (Figure 29). I won’t include everything, so just know that well-placed wrinkles and curves act as valves to help control stool release, blood vessel networks (such as the rectal venous, or hemorrhoidal, plexus) may help pad the stool-passage process, sensitive sensors can detect the difference between solids, liquids, and gases, and various skin configurations provide an appropriate level of toughness, flexibility, and lubrication at the right place and time.
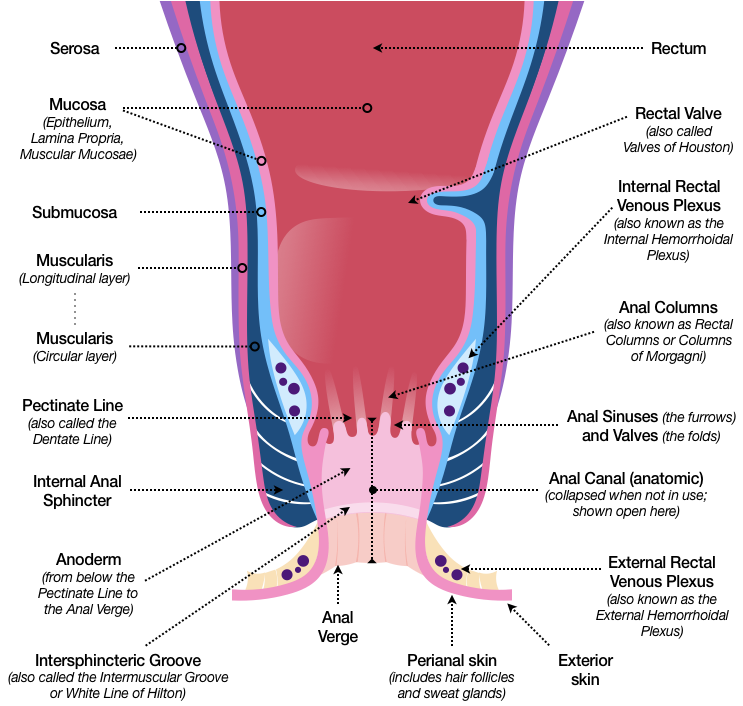
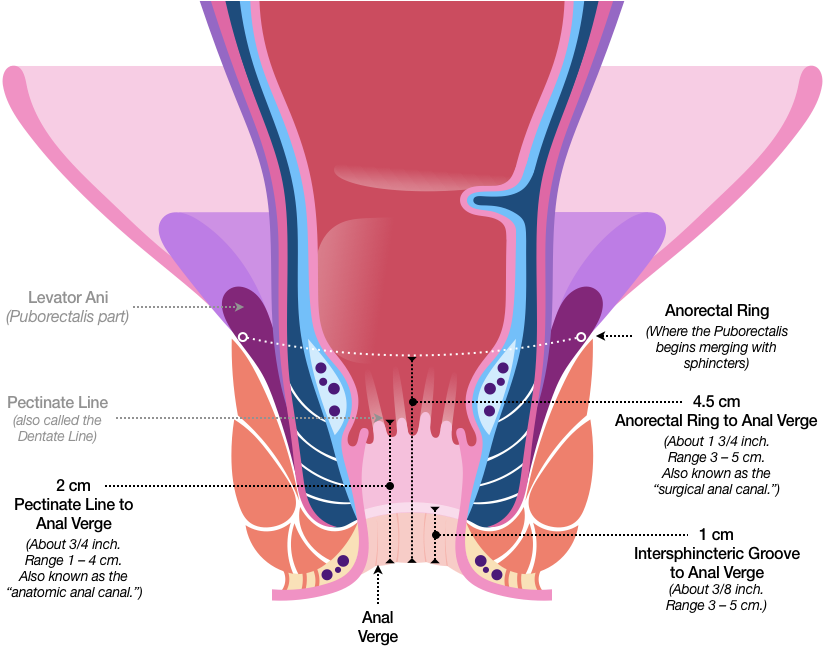
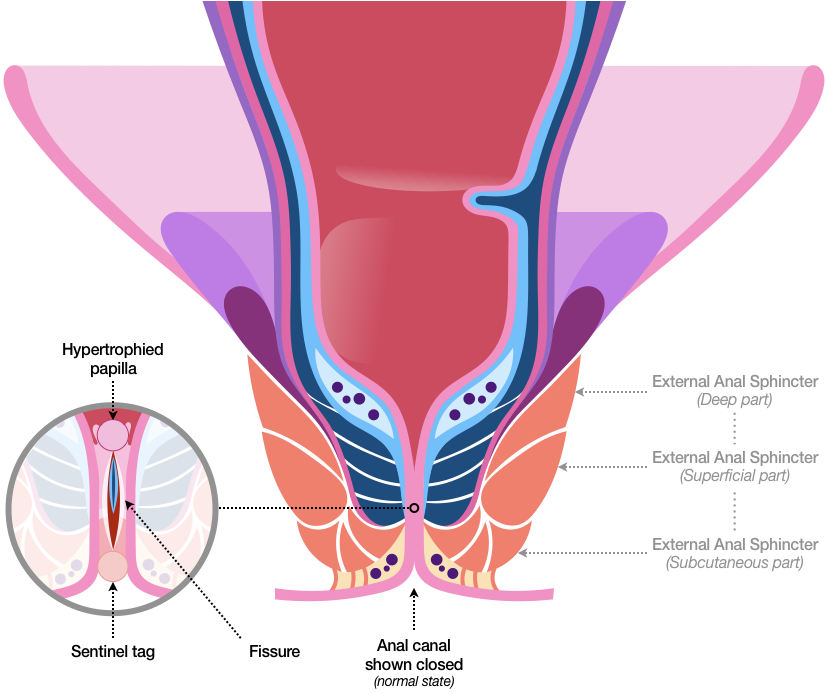
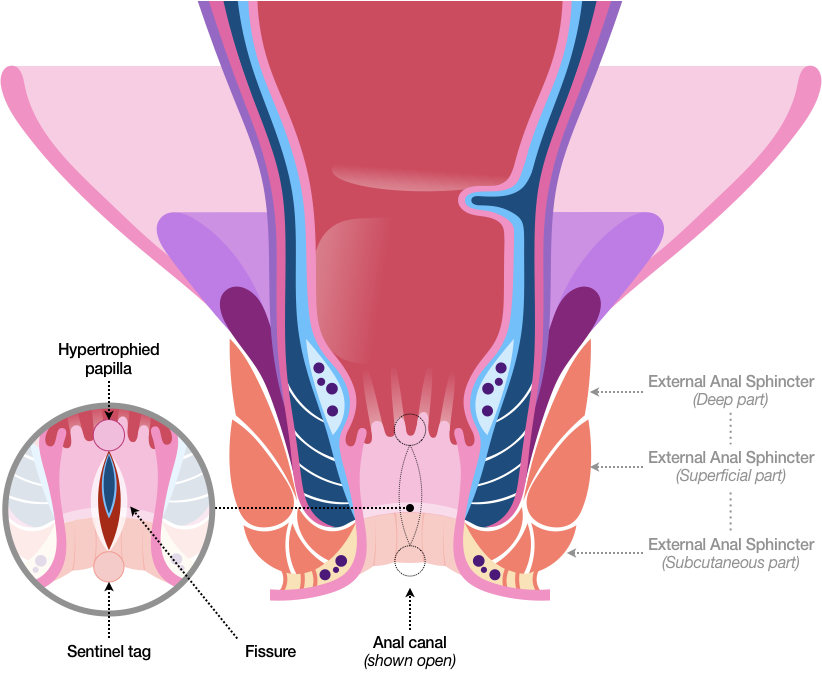
The anal canal specifically, which is measured from different internal starting points based on surgical or functional needs, is home to several specialized tissues responsible for performing a number of complex and coordinated duties. In this sketch, the anal canal is shown open.
Some details:
- Since several features converge at the anal canal, muscle fibers, nerves, and connective tissue intertwine and merge, so remember that this visualization, with its neatly separated areas, is different from reality.
- The innermost red portion represents the lumen and the inner epithelial surface of the mucosa, which is kept moist and lubricated by clear, thin, antiseptic mucus.
- The inner pink-colored sections, which are also part of the mucosa, bunch up in a series of folds, somewhat like a window curtain, at the pectinate line. This area, also called the dentate line (“having teeth or conical projections”), is home to several columns and recesses (sometimes called crypts or sinuses) that house anal glands. Below that is the anoderm (anal skin), which includes a transitional surface area called the pecten, a slight anatomical indentation called the intersphincteric groove (or “intermuscular groove” or “white line of Hilton”), and the anal verge. The anal verge transitions to perianal skin, which then transitions to the familiar epidermis, or exterior skin.
- The light blue layer, the submucosa, houses the internal rectal venous, or hemorrhoidal, plexus, which is a network of blood vessels contained in loose connective tissue.
- The dark blue layer, which represents the circular muscles of the GI wall’s muscularis layer, thickens near the final exit to become the internal anal sphincter.
- Depending on which resource you consult, the longitudinal and serous layers terminate in different places, but usually end up merging with other nearby features in a bundle of muscle or connective tissue.
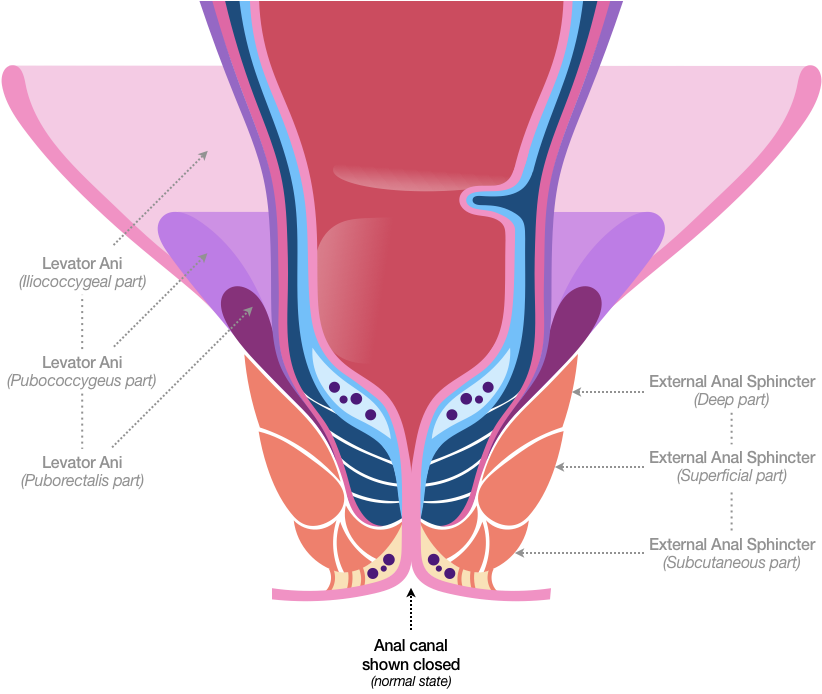
Departing from a strict cross-section view provides some context. The following sketch (Figure 30) shows the anal canal surrounded by all three parts of the fan-shaped levator ani. Remember that the dark purple part of the levator ani muscle—the puborectalis—loops around the anorectal area like a sling.
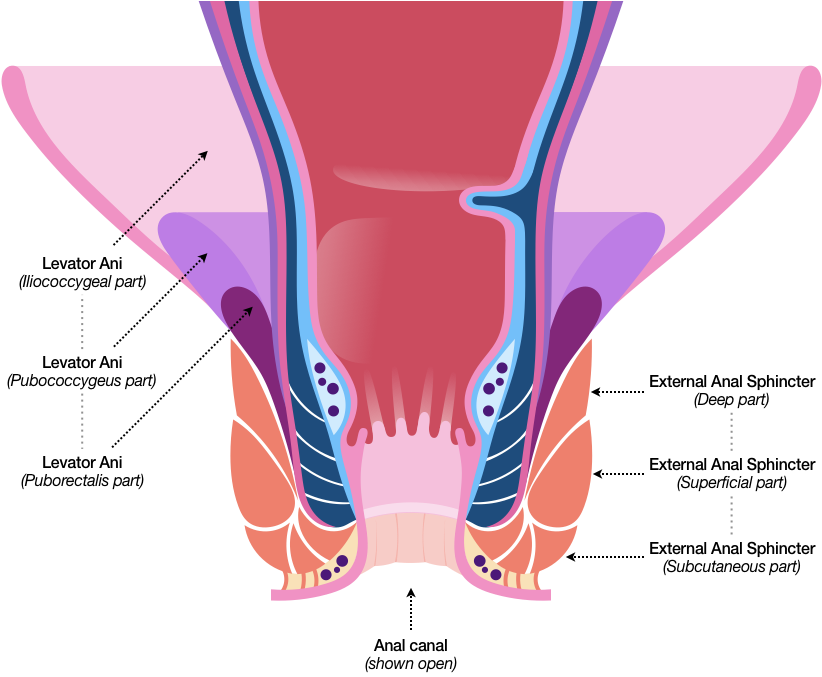
The sketch also adds the external anal sphincter (in orange), which is often described as being made of three parts:
- The deep part appears directly below the levator ani, and merges with the puborectalis muscle (dark purple).
- The superficial part forms the muscular ring (shown earlier) that tightens and loosens around the anal canal.
- The subcutaneous part sits just above the outer network of blood vessels (the external rectal venous, or hemorrhoidal, plexus), and connects to other features, such as the bands of muscle just under the skin (sometimes called the corrugator cutis ani).
This next sketch (Figure 31) also shows the anal canal in an open state, and depicts the location of the anorectal ring, which indicates the place where the puborectalis begins merging with the anal sphincter complex. Also shown are average lengths for the anatomic anal canal (from the pectinate line to the anal verge), and the surgical anal canal (from the anorectal ring to the anal verge).
Before we continue, please focus for a moment on the rectal venous plexus, which includes cross-sectioned veins (depicted as dark purple circles) in the light-blue area. In a few of the references I reviewed, the veins of the rectal venous plexus—thought by some to act like re-inflatable airbags—are shown slightly distending (moving toward the exit) during defecation. This movement seems to have the dual effect of turning the anal crypt openings downward while also covering them protectively. Since the anal crypts contain glands that secrete fluids outward, this natural distention appears to be—from a designer’s perspective—an exceptionally elegant safety feature.
This next sketch (Figure 32) shows the anal canal collapsed, or closed, which is its standard resting state. High muscle tone (tension) at rest may be a contributing factor in multiple anorectal problems.
Since we started this section speaking of cells, let’s now zoom in to the cellular level (Figure 33). As before, I won’t include all the structures. Instead, I’ll focus on the surface cells of the lumen and their gradual transition.
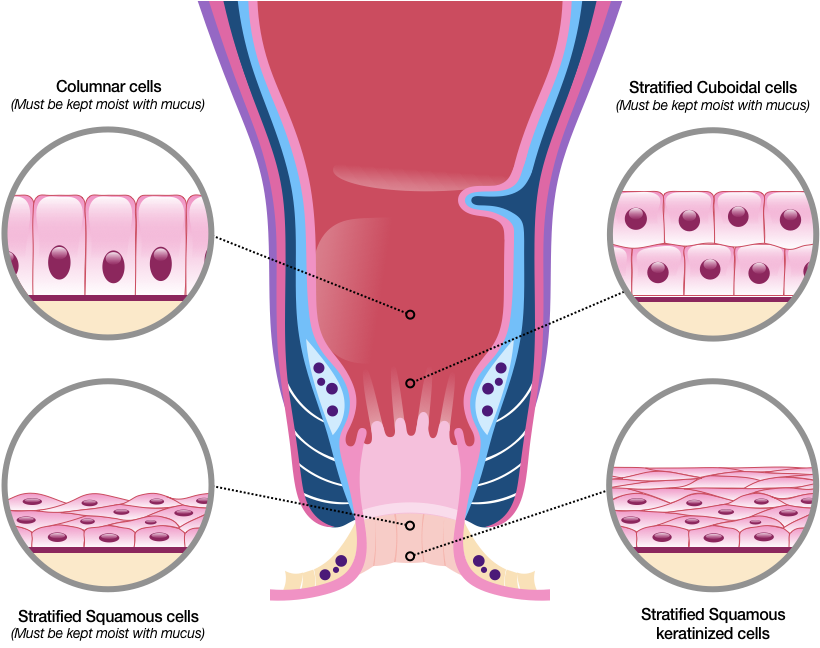
The surface of the GI tract farther away from the anal canal is made mostly of simple columnar epithelium. The column-like structure of these cells promotes absorption and protection, and also helps the GI tract stay lubricated.
Closer to the anal canal (depending on which reference you consult), the simple columnar cells may be accompanied by rows of columnar cells, as well as stacks of cuboidal (cube-like) cells near the anorectal junction at the pectinate line.
The pectinate line marks a transitional space. Below it, squamous (scale-like) epithelial cells take on a flatter, more armor-like structure, and their geometry provides a smooth, abrasion-resistant barrier. Non-keratinized squamous epithelial cells have a nucleus and cytoplasm, and must be kept moist by mucus to avoid drying out.
Keratinized (protein-packed) squamous epithelial cells appear closer to the anal verge. Like exterior skin, the topmost layers lose their nucleus and cytoplasm, and instead get filled with the tough and fibrous protein keratin, which provides waterproofing and even greater protection.
To keep these various cells pliant and effective, and to keep the anal canal functioning optimally, mucus-producing glands are plentiful in this region, as are blood supply and natural sensors. This abundance of features may be one reason a fissure can be so attention-getting. But from my product design perspective, there are at least two other possibilities. Consider:
In humans, the anal canal forms during the fourth to seventh weeks of embryonic development. The pectinate line marks the location where the endoderm—the part of the embryo that turns inward and becomes our GI tract—fuses with cells from a portion of the embryo’s outer surface (the ectodermal proctodeum). Later, the ectoderm on the tube’s other end forms the mouth and merges with the endoderm, which creates a complete GI tract.
This connected tract continues to grow and mature, forming organs, tissues, and cells, including some that would—if not for the help of other features—be destroyed by the very acids they make and release. Similarly, the gastrointestinal wall prevents caustic digestive processes from damaging other internal tissues. Its protection is extensive—if completely stretched out, the GI tract’s epithelium would cover the area of a regulation-size tennis court.
So what does this all this protection suggest?
Technically, it suggests that any material in the lumen is external to the body. Our “inner self” lies between our outer skin and the epithelial cells of our GI tract (Figure 34). In other words, the hollows of our inmost parts actually represent the outside world.
So you see the issue. This highly protective pipeline, built before birth, meets our final outlet at the pectinate line. Thus, any breach in that general area can be interpreted by the body as a significant threat.
A breach can be shallow or deep. For example, erosion and anal rhagades (small linear splits) are shallow losses of epithelial protection. A fissure, by comparison, occurs when part of the anal canal below the pectinate line gets torn or pulled apart forcefully, and the resulting breach can go as deep as the muscle fibers of the internal anal sphincter (Figures 35, 36).
Since all this can happen in a nearly-impossible-to-see waste disposal region, no wonder the body shouts a relentless, painful warning: one of its maximum-security areas has been compromised! So a warning system—that’s the first possibility.
The second possibility comes from me reflecting on my experience long after I healed, and since I can no longer test it under actual conditions, is speculation only…not even a hypothesis. But here’s the general idea in case it might be useful:
Egestion requires coordination among several anorectal features (I’m using the term “egestion” rather than “defecation” to better suggest complex action). As mentioned, the correct egestive act is for the anorectal area to shorten and pull up over exiting material. So it makes good design sense for the areas most likely to bunch, curl, or fold to be very pliant, flexible, and ready to give.
But what would happen if the appropriate muscular movement got incorrectly inverted, forcefully bulging the thinnest and most pliant areas into the anal canal? Structural failure could occur at the weakest point, resulting in a fissure.
If I were designing a recovery process for this possibility, I’d give all built-in healing mechanisms the best chance to do their job by automatically constricting the internal anal sphincter. This would bring the fissure’s edges close together to minimize exposure, reinforce structural integrity, and optimize repair.
I might also signal in urgent, unmistakable terms—perhaps by tightening user-controllable parts of the anorectal area—that the user’s current egestive pattern could cause repeated structural failure if not properly adjusted.
If the error condition continued over time, and if I were unable to communicate clear directions to the user (such as “Stop pushing, straining, and holding your breath, and try a more gentle method”), then I might downgrade entire system performance to encourage more active troubleshooting behavior, somewhat like a computer’s more restrictive “safe mode.”
In this scenario, then, anorectal pain is more than a warning—it’s a direct request for adjustment sent by some internal interface that coordinates and combines involuntary and voluntary healing actions. Since typical digestion also requires handling a complex blend of voluntary and involuntary signals, such an interface doesn’t seem so strange. In fact, modern engineering groups are inventing similar products to monitor critical infrastructure, such as transportation tunnels.
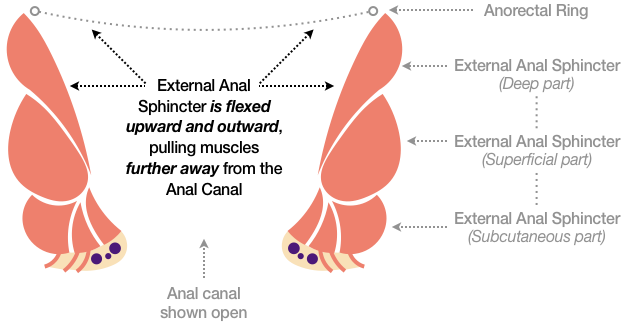
To illustrate this speculation, the following sketches show only the external anal sphincter and the external rectal venous plexus. In the first sketch (Figure 37), the deep, superficial, and subcutaneous parts contract and flex outward, expanding easily into various open spaces that surround the anorectal area, such as the perianal space and the deep postanal space.
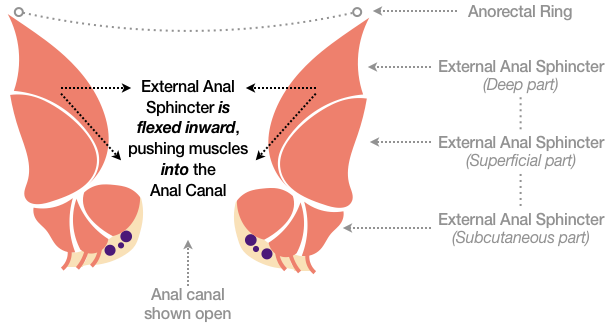
The second sketch (Figure 38) shows the opposite, where the muscles of the external anal sphincter are flexed inward, potentially straining the anorectal area’s most delicate features and bulging them into the anal canal, and perhaps even pinching or damaging veins between the interior and exterior rectal venous plexus. This movement appears to create a high-risk situation, since it both obstructs waste passage and seems prone to structural failure.
Thankfully, the body appears to do its best to minimize danger and damage at both the cellular and structural levels with or without user intervention. For example, granulation tissue, which can fill wounds of almost any size, begins to fill the breach and form a protective barrier in an attempt to help the fissure heal.
I’ll say more about the healing process later, but for now, we can make all this information usable by compressing it down to four key principles:
Follow the food. Overall, what we choose to eat and drink follows a single path. I’ll say more about this in Eating & Drinking, but I found that thinking of my GI tract as one long tube helped me choose what to eat, when to eat, and what to expect as a final result. Cause-and-effect thinking became a powerful ally.
Don’t cross the line. Since our cells quickly transition from tough, keratinized squamous epithelium to less abrasion-resistant types farther up the anal canal, it makes sense to keep any friction-based cleaning routine (such as wiping) a purely external activity. In other words, don’t allow toilet paper or other abrasive materials past the body’s protective exterior surfaces. Hilton’s white line (the intersphincteric groove) marks an easy-to-remember maximum boundary.
Efficient, powerful, and elegant—all the way down. I didn’t know all of the above information while following my protocol, and I got quite an education researching and writing this section. But I knew some things, and as a designer I could both sense and deeply appreciate the GI tract’s remarkably complex simplicity. That deep appreciation is what I’m trying to convey, because acting on it helped me follow the next principle, which changed everything.
Cooperate with the body’s amazing design. Genetic imperfections, developmental defects, and other flaws can happen. An inherited decrease in blood supply to the lower rectal arteries, for instance, can cause healing to take longer, especially for fissures that occur in the posterior midline (back middle) position. But despite personal glitches, when the body’s normal, natural responses are seen in total—attention-getting pain, muscular tightening, and increased fluid flow to flush out toxins, to name a few—an interesting picture begins to emerge. Specifically, the body’s natural mechanisms seem intent on doing the right thing.
I illustrated the GI tract as a series of containers and sphincters to show that most of our functions are handled exceptionally well without conscious thought. The same peristaltic waves that hum along automatically can help waste material exit if given time to act. Clear, thin, antiseptic mucus lubricates and protects the GI tract and helps cleanse it of extraneous material. The entire process, if allowed the freedom to perform its complex combination of chemistry, electricity, physics, and biomechanics, is like a sophisticated, elegant dance. All we need to do is follow along until—briefly—it’s our turn to take a conscious, cooperative lead.
If my short tour wasn’t as clear or thorough as you’d prefer, I hope you can make good use of the keywords and search terms I included in this section as a starting point for your own research. Likewise, finding resources to get a more complete understanding can take a lot of time, so I hope the authoritative sources I used to assemble this content (listed in References) can help you more quickly locate the knowledge you seek.
For now, though, that’s the design of humans. Next, let’s look at design by humans in Functions, Facilities, & Furniture.
Last updated: June 2019